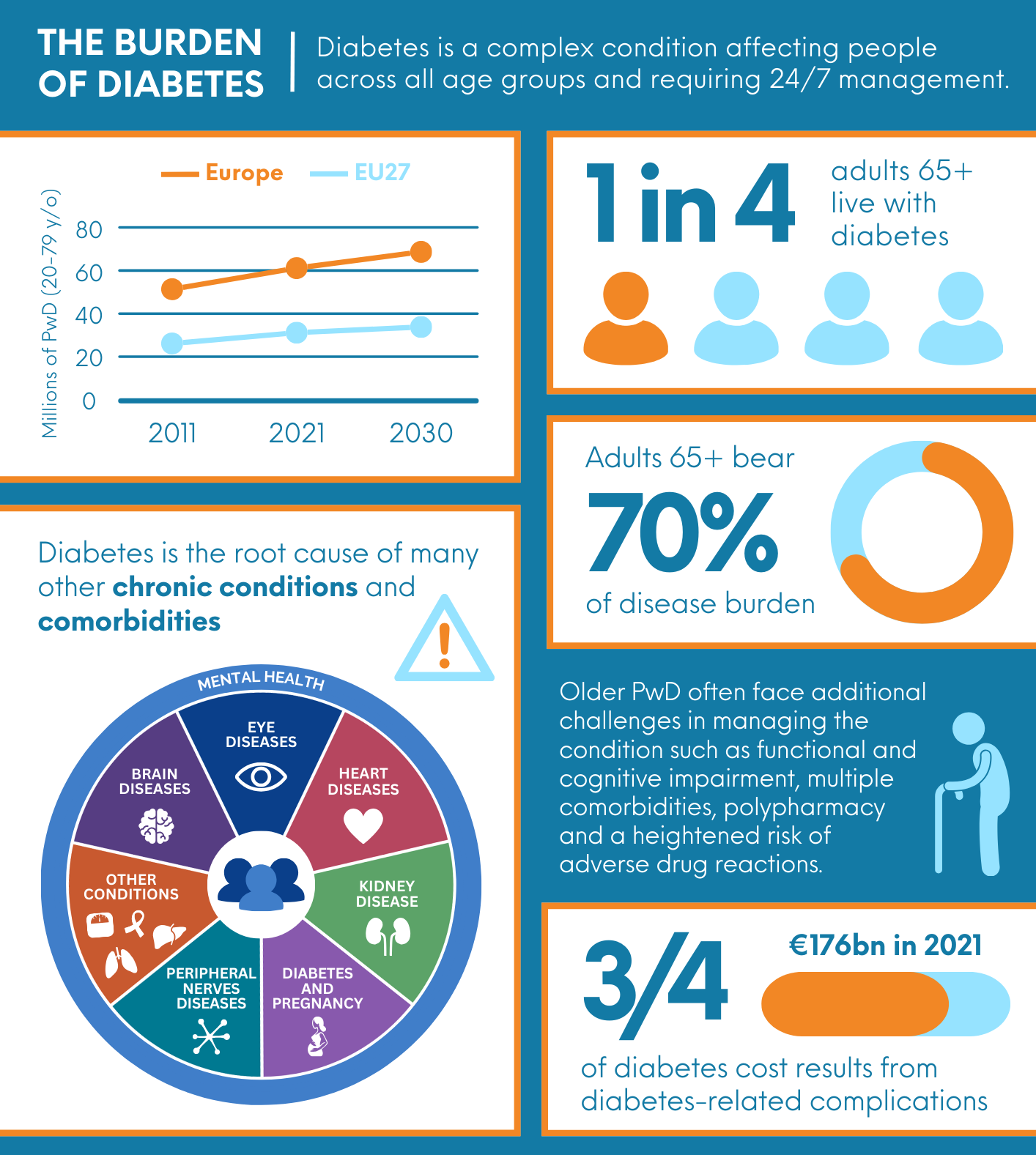
Diabetes is a complex condition affecting people across all age groups, from young individuals to the elderly. It presents a significant global health challenge, contributing to mortality and life-altering complications such as cardiovascular disease (CVD), chronic kidney disease (CKD), lower limb amputations and blindness. In Europe alone, 66 million people live with diabetes, a figure projected to reach 67 million by 2030.
Currently, older adults (>65 years) bear 70% of the disease burden, with one in four living with diabetes. This segment of the population often faces additional challenges in managing the condition such as functional and cognitive impairment, multiple comorbidities, polypharmacy and a heightened risk of adverse drug reactions. These factors make them a distinct group with unique medical needs demanding specialised management and care strategies. However, this population remains largely neglected – a gap that SmartDiabetes seeks to address by recognising and tackling the overlooked challenges older adults with diabetes face.
Of the 24 million older adults living with diabetes in the EU, it is estimated that about half experience some form of functional deterioration, ranging from prefrailty to severe disability. Diabetes, along with its direct and indirect costs, threatens the sustainability and resilience of healthcare systems both in Europe and globally. Among the four leading chronic conditions in Europe – diabetes, heart attack, stroke and cancer – diabetes is the primary driver of the so-called catastrophic healthcare expenditures, defined as costs exceeding 10% of household income per year. The economic burden is immense, with a minimum cost of €72 billion per year, according to an OECD/EU report.
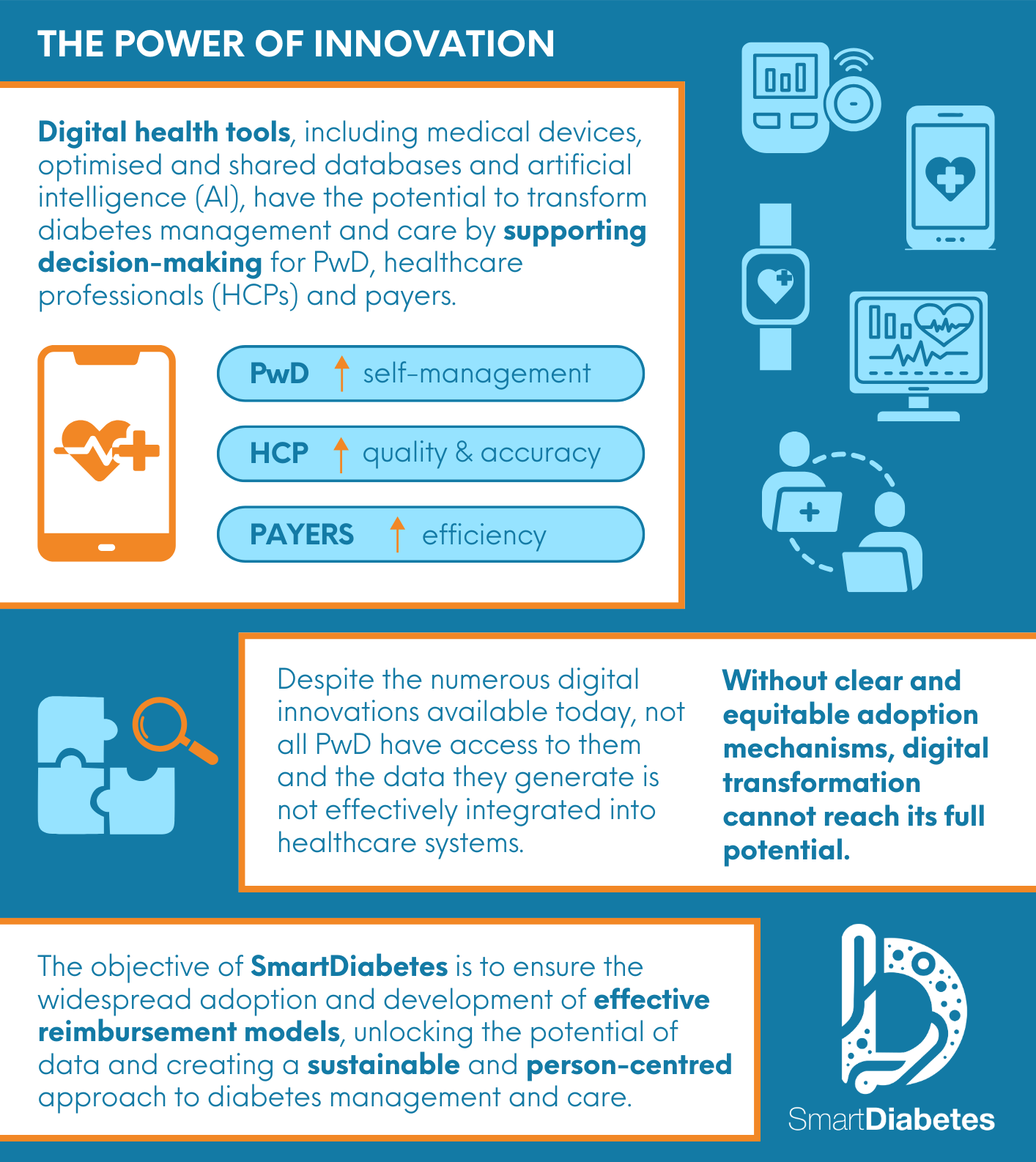
Innovative technological solutions can help alleviate some of these challenges. Digital health tools, including medical devices, optimised and shared databases, and advancements in artificial intelligence (AI), have the potential to transform diabetes management and care. These technologies can support decision-making for PwD (self-management), healthcare professionals (quality and accuracy) and payors (efficiency). However, several obstacles hinder their full potential, including inadequate data integration within healthcare systems, misalignment with clinical workflows, and inconsistent real-world evidence.
Given the escalating costs and the strain on healthcare systems, urgent action is required to ensure that all PwD can manage their condition effectively and achieve the best possible health outcomes.
Over the past decades, numerous technological solutions have been developed to address the complexity of and the gaps in diabetes management. Examples include: continuous glucose monitors (CGMs), connected smart pens and add-ons, such as insulin dosing caps, integrated insulin pumps for precise insulin delivery and mobile apps and platforms for data storage, glucose monitoring and insulin management.
Despite the wealth of digital innovations, the vast amounts of clinical and behavioural data they generate are not effectively integrated into healthcare systems in a comprehensive and actionable manner. As a result, despite promising advancements, data-driven decision-making remains a challenge, making it difficult to implement value-based purchasing models for payers. Without clear adoption mechanisms, the full potential of digital transformation remains unrealised.
While pilot programs and successful case studies exist, systemic adoption at scale has yet to be achieved. The objective of SmartDiabetes is to break this vicious cycle and contribute to ensuring widespread adoption and the development of effective reimbursement models. Unlocking the potential of data is essential to creating a sustainable, efficient and person-centered approach to diabetes management and care.